

Biotech People who develop invasive fungal disease (IFD) often have very non-specific signs and symptoms which makes diagnosis difficult. Additionally, if the diagnosis is delayed, the mortality associated with the IFD increases significantly.
One option is to treat patients with an antifungal before a definite diagnosis and resistance pattern is made using an approach called 'empiric' therapy. Antifungals that have a broad spectrum, are relatively non-toxic and kill fungi can be used empirically, but there are currently limited antifungals available that combine these properties.
BSG005, which has broad spectrum activity including resistant fungal strains, generally good tolerability and kills fungi may be suitable for empiric use. Obtaining a definitive diagnosis can take days or even more than a week, partly because no single diagnostic method is entirely reliable, but also because of the time it takes to send samples to the laboratory, perform the tests and get the results back to the clinician.
Use of empiric antifungals gives the patient the protection of being treated with an antifungal, whilst diagnostic testing takes place.
For diagnosis, samples need to be taken from patients, ideally near the site of the infection, but if the infection is deep in the tissues this can be challenging. Patients who are very sick may have difficulty with their blood forming clots so taking surgical samples or biopsies may not be safe. Other samples such as blood, sputum, urine may not be close to the site of infection and hence are less likely to be sensitive in diagnostic tests, but they are easier to obtain.
A diagnostic sample can be used in various ways to establish the diagnosis. In microscopy and culture, the sample can be spread onto agar plates to attempt to grow the fungus or examined down the microscope with the aim of seeing the fungus (see figure 1), but neither of these methods are very sensitive, so increasingly other methods are used.
These methods fall into two main groups:
Ad 1. Measurement of the patients’ immune response, usually detection of antibodies to the fungus, lacks sensitivity and patients, who are immunocompromised, may be unable to form antibodies. This method, therefore, is often not suited to diagnosis of IFD in very sick patients.
Ad 2. Detection of components of the fungus in samples is the main method currently used for diagnosis. The components, that are detected, are either antigens, which are often pieces of the fungal cell wall, or the genetic material present in the fungus. During fungal growth both antigens and genetic material are released into the patients’ body and detection of them is more sensitive than attempting to grow or visualise the fungus.
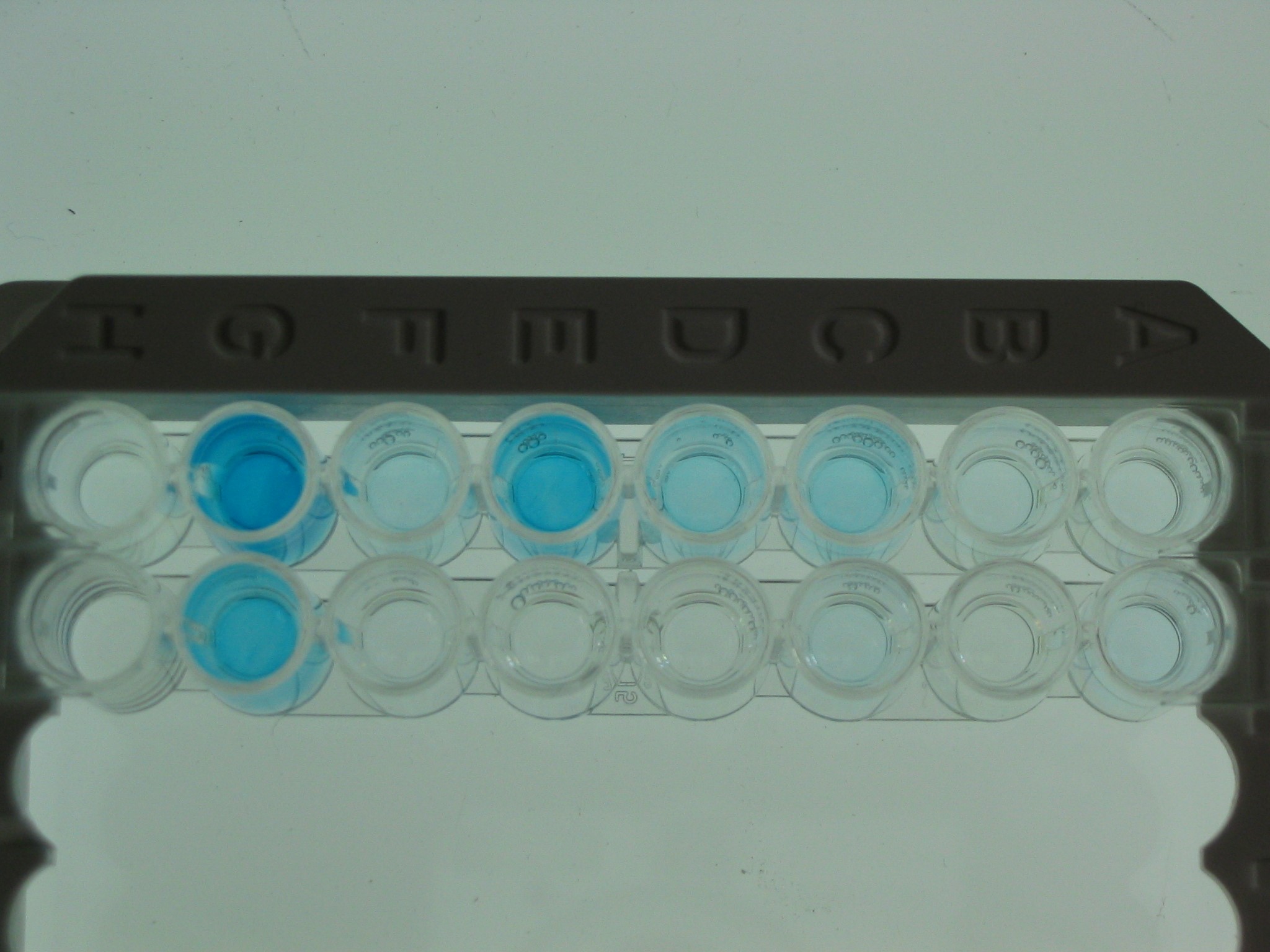
Detection of antigens can often be done in blood or fluid used to ‘lavage’ the bronchia or the lung, avoiding the need for biopsies or surgical samples (see figure 2).
Genetic material from fungi can be detected in a wide range of samples including blood, tissue, sputum and many more. The sensitivity of these methods does vary depending on the patients’ underlying disease, but is much better than microscopy and culture.
Obtaining a definitive diagnosis of IFD continues to be a challenging and time-consuming process despite advances in the methods available. The lack of specific signs and symptoms of IFD, the difficulties in obtaining suitable samples, the low sensitivity of some diagnostic tests, time to find any resistance pattern, the length of time to receive results after testing and significant variability in access to relevant diagnostic laboratory facilities all contribute to the challenge.
Use of an empiric antifungal, including potentially BSG005, can give patients valuable protection until the diagnosis can be made.
Images:
Figure 1. Fungus in a sample from a patient with an IFI seen down the microscope. The sample has been stained and the fungus looks fluorescent using a specific microscope with appropriate filters
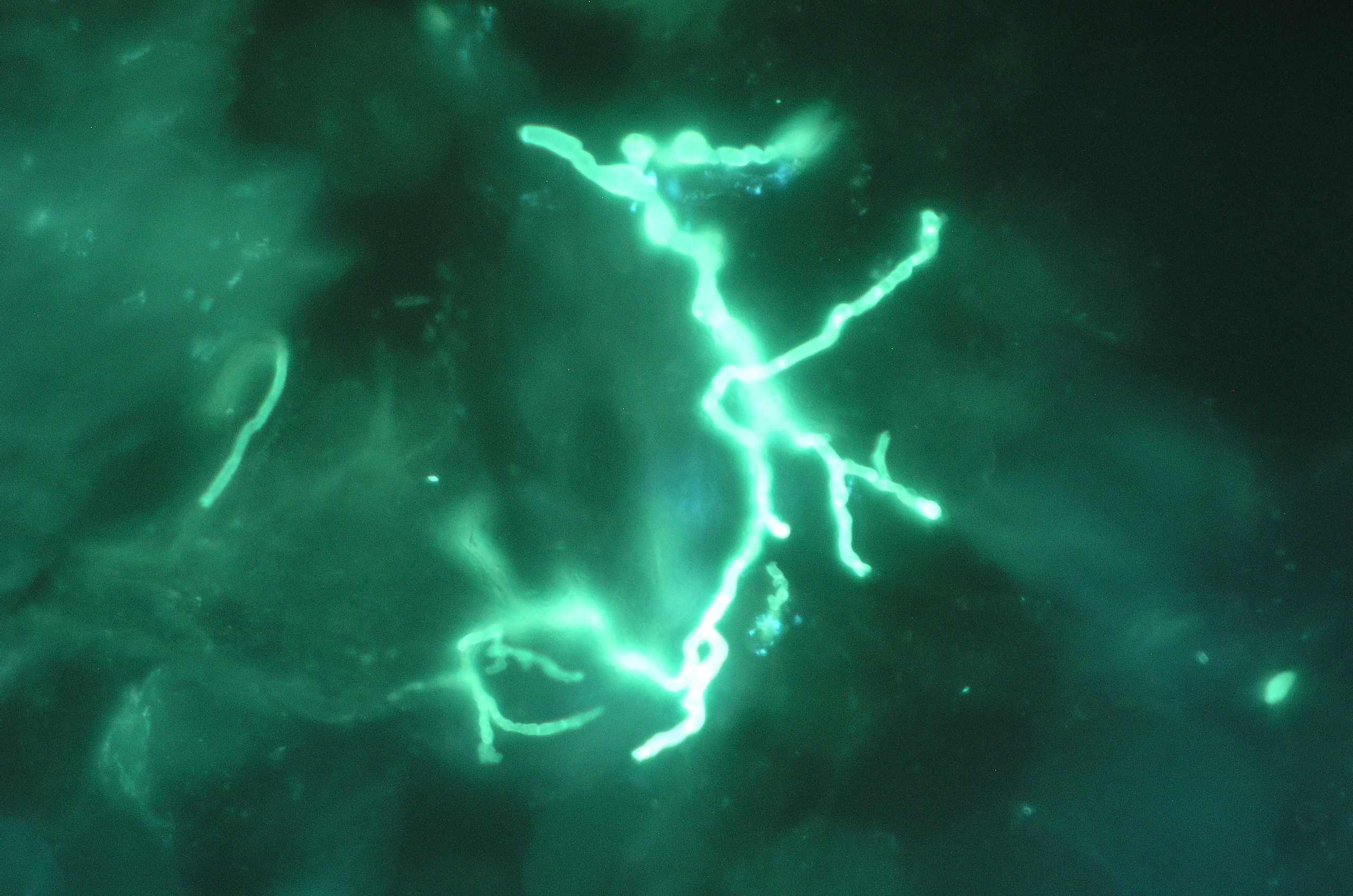
Figure 2. Detection of fungal antigen. The top row contains control samples and the lower row contains a positive sample (blue well) from a patient with an IFI.
Ruth Ashbee PhD
Fellow of the European Confederation of Medical Mycology
Det här är en sponsrad artikel framtagen i samarbete med Biosergen. Sponsrade inlägg är en del av Börsvärldens annonserbjudande. Om du med anledning av våra sponsrade inlägg önskar att komma i kontakt med oss, vänligen skriv till IR@borsvarlden.com.
LÄS MER